Vaccination disparities risk further entrenching disadvantage

Sydney’s lockdown ends on Monday and Melbourne follows later this month, with fully vaccinated people gaining a number of social and economic privileges not available to those who are yet to be vaccinated.
Freedoms for those who are double-vaccinated will vary between states, but include greater access to employment, education and other activities, such as having visitors in your home, going shopping or going to the gym.
With vaccination rates generally lower among low socioeconomic groups, this is likely to further increase the inequality between the most and least socioeconomically advantaged Australians.
Australia faces two main COVID challenges: how to increase vaccination rates in priority populations and how to continue to protect these groups.
How vaccination rates compare
This week’s vaccination data by local government area (LGA) in Victoria show continued uptake of COVID-19 vaccination in most government areas.
The graph below shows the distribution of first and second doses, as well as the required percentage to reach 95% full coverage, in the three most and three least socioeconomically disadvantaged LGAs.
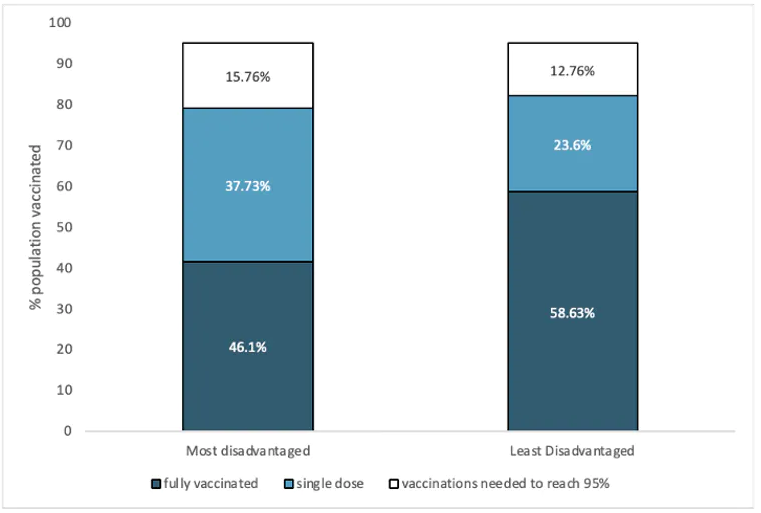
Vaccination rates, comparison between least (Brimbank, Greater Dandenong and Hume) and most socioeconomically advantaged LGAs (Stonnington, Broondara and Glen Eira) in Metro Melbourne. It shows double dose vaccination rates at 46.1% for the most disadvantaged and 58.65 for the least disadvantaged. ABS
Sydney reports a similar distribution between low and high socioeconomic LGAs but is ahead of Melbourne in overall vaccination rates.
Pandemic of the poor & disadvantaged
COVID-19 is quickly becoming a pandemic of the poor and disadvantaged. Four times as many poorer Australians died of COVID in 2020 than those from wealthier backgrounds.
COVID infection rates are higher where there are higher numbers of essential workers, larger family groups under one roof, and people living in shared homes.
This trend is also seen in a range of other countries, including Chile and Israel.
Indigenous Australians have one of the highest risks of dying from COVID-19. At the end of September, just 30% of First Nations Australians were fully vaccinated, despite being a priority population. Currently this rate is at 41%, showing progress but still insufficient protection.
Disability advocates have warned Australia could face a similar situation to the United Kingdom, where 60% of people who died from COVID had a disability.
As of September 15, only 40% of NDIS participants were fully vaccinated, despite also being a priority population.
New disease, but old health problems
Disadvantaged groups are much more likely to suffer one or more chronic illness such as diabetes, heart disease and lung disease. These conditions put them at higher risk of severe illness or death if they contract COVID.
These underlying health conditions mean the poorest 20% of Australians die up to 6.4 years earlier than the wealthiest 20%.
People with a severe mental illness die up to 23 years earlier, mostly due to physical ill health.
Poor and disadvantaged Australians are also at greatest risk of getting COVID and becoming seriously ill.
Yet the modelling for easing restrictions does not take into account how “opening up” will affect these groups.
Our health and recovery policies must not leave these groups behind. Targeted and bespoke information and services are needed for disadvantaged Australians to overcome these barriers.
So what needs to happen?
COVID cases are expected to rise when restrictions are lifted and public health measures eased. This will leave vulnerable groups at greater risk of COVID.
As other researchers have argued, in addition to high overall vaccination targets, preventing further lockdowns will require a layered plan that includes:
- specific vaccine targets for priority populations
- making indoor air safer
- maintaining high rates of testing and tracing
- booster shots.
Such a layered plan combined with staggered lifting of restrictions is critical to prevent high case numbers and potential severe illness and deaths in populations already disproportionately affected by other health conditions.
We also need to boost the health literacy of disadvantaged Australians so they can better understand and have greater confidence in the information about their health in general, including in relation to COVID and beyond.
Stella McNamara, research assistant at the Mitchell Institute, co-authored this article![]()
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Australia's health tracker by socio-economic status
Report
Many children with disability struggle to get an appointment, despite being priority
The Conversation
Vaccinations need to reach 90% of First Nations adults and teens
The Conversation
Relying only on vaccination in NSW isn’t enough – here’s what we need for sustained freedom
The Conversation



